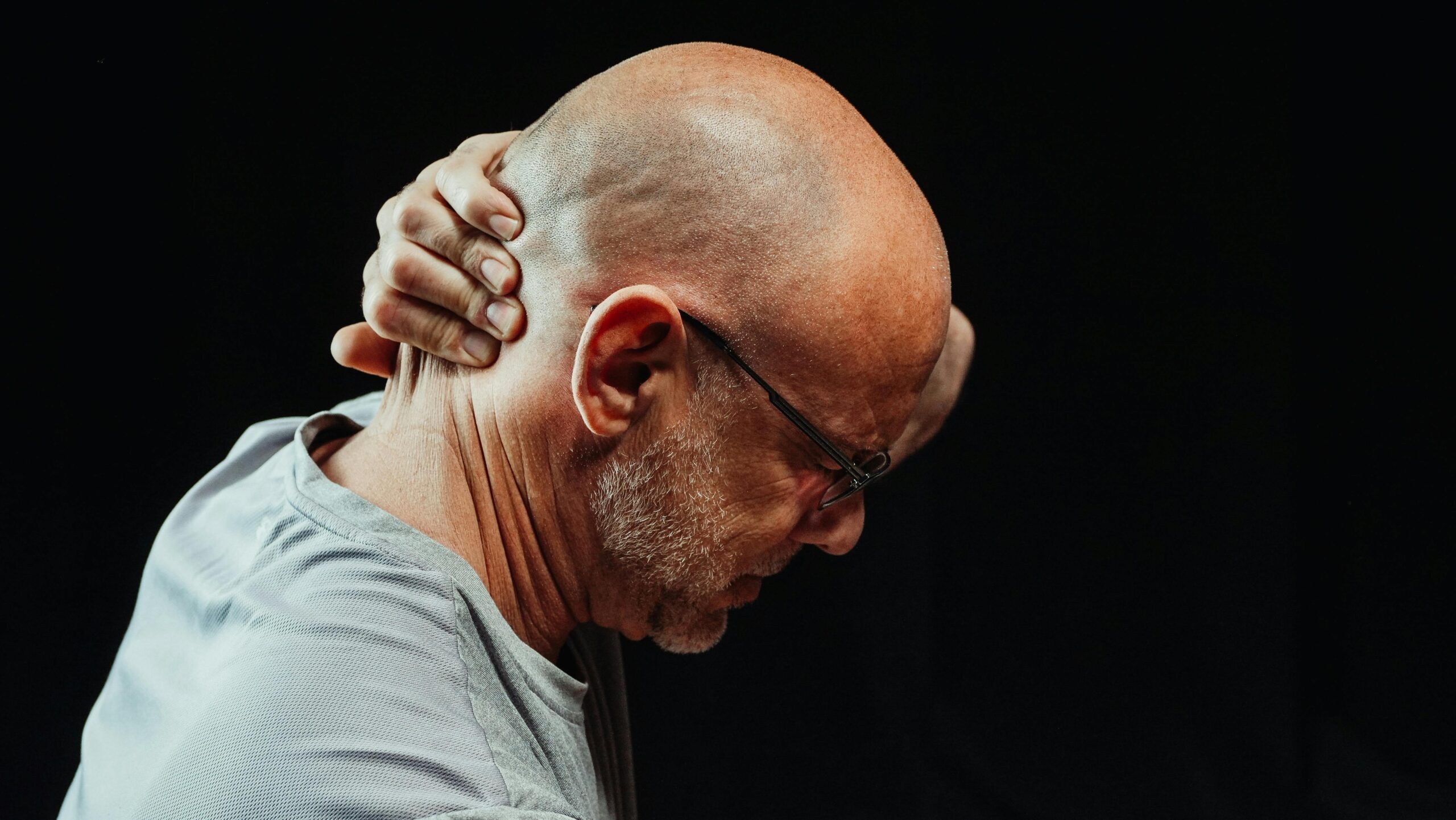
Living with chronic pain doesn’t mean accepting a sedentary life. Gentle low-load strengthening exercises can transform your experience with persistent discomfort, offering a path toward improved mobility and lasting relief.
For millions worldwide, chronic pain has become an unwelcome companion that dictates daily activities, limits movement, and diminishes quality of life. The traditional approach of complete rest or avoiding physical activity often backfires, leading to muscle weakness, joint stiffness, and ironically, more pain. However, emerging research and clinical practice demonstrate that carefully designed low-load strengthening routines can break this cycle, empowering individuals to reclaim their bodies and their lives without aggravating existing conditions.
🔍 Understanding the Connection Between Weakness and Chronic Pain
Chronic pain and muscle weakness exist in a vicious cycle that perpetuates suffering. When we experience pain, our natural instinct is to protect the affected area by limiting movement. This protective behavior, while initially helpful for acute injuries, becomes problematic when extended over weeks, months, or years.
The muscles surrounding painful joints or regions begin to atrophy from disuse. Weaker muscles provide less support to joints and the skeletal system, placing additional stress on already sensitive tissues. This increased mechanical stress intensifies pain signals, which in turn discourages movement even further. Understanding this relationship is the first step toward breaking free from the pain cycle.
Research published in pain management journals consistently shows that appropriate strengthening exercises can interrupt this negative feedback loop. By gradually rebuilding muscular support systems, we reduce mechanical stress on painful structures and improve the body’s natural pain-modulating mechanisms.
Why Low-Load Training Works for Chronic Pain Conditions
Low-load strengthening differs fundamentally from traditional resistance training. Instead of lifting heavy weights to build maximum strength or muscle size, low-load exercises use minimal resistance combined with controlled movements and higher repetitions. This approach offers several advantages for people managing chronic pain.
First, low loads minimize the risk of pain flare-ups. Heavy resistance can trigger protective muscle guarding and exacerbate inflammation in sensitive tissues. Light loads allow the nervous system to remain calm, reducing the likelihood of pain amplification during and after exercise.
Second, this approach emphasizes motor control and movement quality over pure strength. Many chronic pain conditions involve dysfunctional movement patterns where certain muscles become overactive while others remain inhibited. Low-load exercises provide an ideal environment for retraining these patterns without overwhelming the system.
Finally, low-load training proves more sustainable for long-term adherence. People with chronic pain can perform these exercises more frequently without extended recovery periods, building consistency—the true foundation of lasting improvement.
🎯 Essential Principles for Pain-Friendly Exercise
Before diving into specific exercises, understanding key principles ensures your strengthening routine supports healing rather than causing setbacks.
Start Exceptionally Low and Progress Gradually
Your starting point should feel almost too easy. This isn’t laziness—it’s strategic. Beginning with minimal challenge allows your nervous system to adapt without triggering protective pain responses. Consistency matters more than intensity in the early stages of pain rehabilitation.
Progress should be measured in weeks, not days. Increasing difficulty by just 10% per week gives tissues adequate time to adapt while building confidence in your body’s capabilities.
Respect Pain Signals Without Fear
Not all pain during exercise indicates harm. Learning to distinguish between discomfort from muscle effort and pain signaling tissue damage is crucial. A general guideline: discomfort that remains below 3-4 on a 10-point scale and resolves within two hours post-exercise is typically acceptable.
Pain that sharply increases during movement, persists significantly after exercise, or worsens over subsequent days suggests you’ve exceeded current tolerance. This isn’t failure—it’s valuable information guiding adjustments to your routine.
Prioritize Consistency Over Intensity
Five minutes of gentle exercise performed daily produces superior results compared to intense 45-minute sessions once weekly. Frequent, low-dose movement exposure helps desensitize painful areas and builds neural pathways for improved motor control.
Building Your Foundation: Core Low-Load Exercises 💪
These foundational movements target common areas affected by chronic pain while remaining accessible to most individuals. Each can be modified to match current capabilities.
Modified Glute Bridges for Lower Back and Hip Pain
Lie on your back with knees bent and feet flat on the floor, hip-width apart. Gently press through your heels to lift your hips just a few inches off the ground—not seeking maximum height, but rather focusing on feeling the gluteal muscles engage. Hold for 3-5 seconds, then lower slowly.
Begin with 8-10 repetitions, performing 2-3 sets. This exercise strengthens the posterior chain while minimizing spinal compression, making it ideal for lower back pain management.
Wall Push-Ups for Upper Body Strength
Stand facing a wall, arms extended at chest height with palms flat against the surface. Position feet far enough back that you feel gentle tension but can maintain proper form. Bend elbows to bring your chest toward the wall, then press back to starting position.
This vertical variation eliminates gravitational load while building shoulder, chest, and arm strength. Perform 10-15 repetitions for 2-3 sets, focusing on controlled movement quality.
Seated Knee Extensions for Knee Pain
Sit in a sturdy chair with feet flat on the floor. Slowly extend one knee until the leg is straight (or as far as comfortable), hold for 2-3 seconds, then lower with control. This simple movement strengthens the quadriceps muscle, which is critical for knee joint stability and pain reduction.
Complete 10-12 repetitions per leg for 2-3 sets. If straightening completely causes discomfort, work within a smaller, pain-free range of motion.
Shoulder Blade Squeezes for Neck and Upper Back Tension
Sit or stand with arms relaxed at your sides. Gently draw your shoulder blades together, as if squeezing a pencil between them, without shrugging shoulders toward ears. Hold for 5 seconds, then release.
This exercise activates the middle trapezius and rhomboid muscles, which often become weak in people with chronic neck and upper back pain. Perform 12-15 repetitions, 2-3 times throughout the day.
Gentle Calf Raises for Ankle and Foot Issues
Stand near a wall or counter for light support. Rise onto the balls of your feet, lifting heels 1-2 inches off the ground, hold briefly, then lower with control. This strengthens the calf muscles and improves ankle stability.
Begin with 10-12 repetitions for 2 sets. If balance is challenging, maintain light fingertip contact with your support surface throughout the movement.
📅 Creating Your Weekly Strengthening Schedule
Structure enhances adherence and ensures balanced development without overtraining any single area. Here’s a practical weekly framework adaptable to various chronic pain conditions:
| Day | Focus Area | Duration | Exercises |
|---|---|---|---|
| Monday | Lower Body | 10-15 minutes | Glute bridges, knee extensions, calf raises |
| Tuesday | Upper Body | 10-15 minutes | Wall push-ups, shoulder squeezes |
| Wednesday | Active Rest | 5-10 minutes | Gentle stretching or walking |
| Thursday | Lower Body | 10-15 minutes | Glute bridges, knee extensions, calf raises |
| Friday | Upper Body | 10-15 minutes | Wall push-ups, shoulder squeezes |
| Weekend | Flexible | 5-15 minutes | Light activity or rest as needed |
This schedule provides adequate recovery between sessions targeting the same muscle groups while maintaining movement frequency throughout the week. Adjust based on individual response and specific pain patterns.
Progressing Safely: When and How to Advance Your Routine
Knowing when to increase difficulty prevents both stagnation and overexertion. Several indicators suggest readiness for progression:
- Exercises feel significantly easier than when you started
- You complete all sets without pain increases
- Recovery between sessions feels complete
- Daily pain levels have decreased or stabilized
- You’ve maintained current difficulty for at least 2-3 weeks
When these conditions align, advance using one of these strategies:
Increase Repetitions First
Before adding resistance, increase repetitions by 2-3 per set. This builds endurance and confirms tissue tolerance before intensifying load.
Add Extra Sets Gradually
If performing two sets comfortably, add a third set to one exercise per session. Monitor response over the following week before adding more volume.
Introduce Light Resistance Carefully
After mastering bodyweight variations, incorporate resistance bands or light weights (1-3 pounds initially). The added resistance should feel noticeable but not challenging enough to compromise movement quality.
Progress Movement Difficulty
Advance to more challenging variations: wall push-ups become counter push-ups, then knee push-ups. Each progression changes biomechanics and increases load while remaining within low-load parameters.
🧘 Complementary Strategies That Enhance Results
While low-load strengthening forms the foundation, integrating complementary approaches accelerates improvements and addresses multiple dimensions of chronic pain.
Breathing Techniques for Nervous System Regulation
Chronic pain often maintains the nervous system in a heightened threat state. Diaphragmatic breathing before, during, and after exercise activates parasympathetic responses that reduce pain sensitivity and muscle tension.
Practice inhaling for 4 counts through your nose, allowing your belly to expand, then exhaling for 6 counts through pursed lips. Perform 5-10 breath cycles before beginning your strengthening routine.
Movement Throughout the Day
Formal exercise sessions matter, but micro-movements throughout the day prevent prolonged static postures that increase pain. Set hourly reminders for 1-2 minute movement breaks: shoulder rolls, gentle twists, brief walks, or standing stretches.
Sleep Optimization
Quality sleep profoundly influences pain perception and tissue recovery. Establish consistent sleep-wake times, create a cool, dark sleeping environment, and avoid screens for 60 minutes before bed. Adequate rest amplifies benefits from your strengthening routine.
Tracking Progress Objectively
Chronic pain can distort perception of progress. Maintain a simple log tracking exercise completion, pain levels, and functional abilities. Review monthly to recognize improvements that might otherwise go unnoticed, providing motivation during challenging periods.
Overcoming Common Obstacles and Setbacks 🛠️
The path from chronic pain to improved function rarely follows a straight line. Anticipating challenges prepares you to navigate them effectively.
Managing Pain Flare-Ups
Despite careful progression, occasional flare-ups occur. Rather than abandoning your routine entirely, scale back to earlier, more comfortable exercise variations. Maintain movement at reduced intensity rather than complete rest, which often prolongs recovery.
Addressing Motivation Fluctuations
Motivation naturally ebbs and flows. Build systems that support consistency regardless of motivation levels: exercising at the same time daily, preparing your space in advance, or partnering with an accountability buddy. Action creates motivation more reliably than waiting for inspiration.
When Professional Guidance Becomes Necessary
While self-directed low-load strengthening helps many individuals, certain situations warrant professional evaluation:
- Pain progressively worsening despite conservative approaches
- New neurological symptoms like numbness, tingling, or weakness
- Pain accompanied by unexplained weight loss or fever
- Inability to find any exercises that remain tolerable
- Uncertainty about proper exercise selection or technique
Physical therapists specializing in chronic pain can provide personalized assessment, hands-on treatment, and customized exercise progressions that accelerate recovery.
Real-World Success: What to Expect Over Time ⏰
Understanding realistic timelines prevents discouragement and celebrates incremental victories along the recovery journey.
During the first 2-4 weeks, many people notice improved confidence and reduced fear around movement, even if pain levels remain unchanged. This psychological shift matters tremendously, as fear avoidance significantly contributes to disability in chronic conditions.
Between weeks 4-8, subtle physical improvements emerge: slightly increased range of motion, reduced muscle guarding, or better tolerance for daily activities. Pain may still fluctuate but typically with reduced intensity and duration.
After 8-12 weeks of consistent practice, more substantial changes become apparent. Strength gains translate into functional improvements—standing longer, walking farther, or performing previously difficult tasks with less discomfort. Pain often becomes less central to daily experience.
Beyond three months, continued adherence maintains gains and allows progressive advancement toward more challenging activities. Many individuals find that exercise transforms from a pain management obligation into an enjoyable component of their lifestyle.
Building Long-Term Resilience Beyond Pain Relief
The ultimate goal extends beyond simply reducing pain. Low-load strengthening cultivates resilience—the capacity to adapt to stress, recover from setbacks, and maintain function despite challenges.
This resilience develops through consistent practice that proves to your nervous system that movement is safe, your body is capable, and discomfort doesn’t necessarily signal danger. Over time, this reconditioning reduces central sensitization, where the nervous system amplifies pain signals disproportionately to tissue state.
Additionally, the discipline and body awareness developed through regular exercise enhance overall health behaviors. Improved strength supports better posture, reduces fall risk, maintains bone density, and contributes to cardiovascular health—benefits extending far beyond pain management.
Your First Step Toward Transformation Starts Today 🌟
Chronic pain may have limited your life until now, but gentle low-load strengthening offers a practical, accessible path toward reclaiming mobility and reducing suffering. The exercises outlined here require no special equipment, minimal time investment, and can be adapted to virtually any current ability level.
Begin where you are, not where you think you should be. Select just two or three exercises that feel manageable, perform them for five minutes daily, and observe what happens. Small, consistent actions compound over weeks and months into transformative results.
Remember that setbacks don’t erase progress—they’re part of the process. Each time you return to your routine after a difficult day, you build both physical strength and mental resilience. You’re not just exercising; you’re rewriting your relationship with your body and demonstrating that chronic pain doesn’t define your capabilities.
The journey from chronic pain to improved function requires patience, self-compassion, and persistence. But unlike passive treatments that provide temporary relief, low-load strengthening empowers you to become an active participant in your own recovery. Your future self—more mobile, more confident, and less limited by pain—will thank you for starting today.
Toni Santos is a movement specialist and pain recovery educator focused on managing chronic foot and lower limb conditions through progressive mobility strategies, informed footwear choices, and personalized walking progression. Through a practical and body-centered approach, Toni helps individuals rebuild confidence, reduce flare-ups, and restore function using evidence-based movement routines and environmental adaptation. His work is grounded in understanding pain not only as a sensation, but as a signal requiring strategic response. From flare-up calming techniques to surface strategies and graduated activity plans, Toni delivers the practical and accessible tools through which people reclaim mobility and manage their symptoms with clarity. With a background in rehabilitation coaching and movement education, Toni blends biomechanical awareness with real-world guidance to help clients strengthen safely, walk smarter, and choose footwear that supports recovery. As the creator behind Sylvarony, Toni develops structured recovery frameworks, progressive walking protocols, and evidence-informed routines that empower people to move forward with less pain and more control. His work is a resource for: Managing setbacks with the Flare-up Management Toolkit Making smart choices via the Footwear and Surface Selection Guide Building endurance through Graded Walking Plans Restoring function using Mobility and Strengthening Routines Whether you're recovering from injury, managing chronic foot pain, or seeking to walk with less discomfort, Toni invites you to explore structured pathways to movement freedom — one step, one surface, one strengthening session at a time.




